Every year, millions of older adults suffer falls that can quickly turn deadly or life-changing. What many don’t realize is that after age 65, even a seemingly minor slip can result in devastating injuries or long-term complications. This isn’t just bad luck—there’s a complex web of biological, neurological, and environmental factors at play, silently increasing risk as we age. Understanding the hidden science behind balance and falls is crucial, not just for seniors, but for everyone who cares about aging well and safely.
1. The Anatomy of Balance

Balance is a delicate process, relying on the vestibular system in the inner ear, our vision, and proprioception—the body’s sense of position.
As we age, each of these systems may decline: inner ear structures stiffen, vision blurs, and nerve signals slow.
This cumulative degeneration can make it much harder to stay upright and react to sudden changes.
According to Johns Hopkins Medicine, these subtle losses often go unnoticed—until a fall occurs.
2. Bone Density Decline

After age 65, bone density loss accelerates, leaving bones more fragile and prone to fractures during a fall.
Women typically experience faster bone loss than men, especially post-menopause, making them particularly vulnerable.
Osteoporosis—often called the “silent disease”—can progress unnoticed until a serious break occurs.
The National Institutes of Health warns that weakened bones dramatically increase the severity of injuries from even minor tumbles, turning a simple fall into a life-altering event.
3. Slower Reflexes and Reaction Time

Aging brings a noticeable slowdown in neuromuscular response, making it harder for seniors to react quickly when they stumble.
Whereas younger adults might instinctively brace themselves, older adults often can’t respond in time.
According to Harvard Health, average reaction times are significantly slower in those over 65, increasing the likelihood of a direct and dangerous fall.
4. Weaker Muscles and Sarcopenia

With age, many adults develop sarcopenia—the gradual loss of muscle mass and strength.
This condition makes it harder to maintain good posture, walk steadily, or recover quickly from a misstep.
Weak muscles reduce stability and increase the effort needed to avoid a fall.
The Mayo Clinic highlights sarcopenia as a key driver of frailty, making falls both more likely and more severe for older adults.
5. Vision Changes

As we age, conditions like cataracts and macular degeneration become common, blurring vision and distorting depth perception.
These impairments make it harder to spot obstacles or judge steps accurately.
According to the American Academy of Ophthalmology, seniors with visual impairment experience falls at twice the rate of those with healthy vision, showing just how critical eyesight is to staying safe.
6. Inner Ear Disorders

Disorders of the inner ear, especially benign paroxysmal positional vertigo (BPPV), frequently cause sudden dizziness or a spinning sensation.
These balance disruptions make walking or even standing hazardous.
The Cleveland Clinic notes that older adults are far more likely to develop these conditions, which can dramatically increase their risk of falls and related injuries.
7. Medication Side Effects

Many seniors take multiple medications—known as polypharmacy—for chronic conditions.
Common drugs like blood pressure medications and sedatives can trigger dizziness, low blood pressure, or drowsiness, all of which undermine balance and alertness.
Studies show that those on several medications face a significantly higher fall risk compared to those taking just one.
The CDC warns that reviewing medications regularly is essential for minimizing these hidden dangers.
8. Chronic Illnesses

Chronic illnesses such as diabetes, arthritis, and Parkinson’s disease can seriously compromise balance and mobility.
Nerve damage from diabetes, joint stiffness from arthritis, or tremors from Parkinson’s all disrupt the body’s ability to stay steady.
The National Council on Aging reports that older adults with chronic conditions experience much higher fall rates, making disease management a crucial part of fall prevention.
9. Blood Pressure Fluctuations

Many older adults experience orthostatic hypotension, a sudden drop in blood pressure when rising from a chair or bed.
This can cause unexpected dizziness, lightheadedness, or even fainting—leading directly to falls.
The American Heart Association highlights that these blood pressure swings are especially common in those over 65, further stacking the odds against safe mobility.
10. Slower Healing and Recovery

As we age, the body’s ability to heal slows considerably.
Fractures and wounds that might mend in weeks for younger adults can take months for seniors, often requiring extended hospitalization.
This delay not only increases the risk of complications like infections but can also lead to lasting disability.
The NIH underscores that slow recovery amplifies the overall danger of falls in those over 65.
11. Reduced Sensation in Feet

Conditions such as peripheral neuropathy—often linked to diabetes—can cause numbness or tingling in the feet.
This loss of sensation makes it difficult to sense uneven surfaces, obstacles, or changes in ground texture, undermining balance.
The American Diabetes Association notes that diminished foot sensation is a key reason older adults are more prone to tripping and falling.
12. Joint Stiffness and Limited Mobility

Aging often brings osteoarthritis and cartilage loss, leading to stiff, painful joints.
This stiffness can make it difficult to react quickly or adjust posture to avoid a fall.
According to the Arthritis Foundation, older adults with arthritis are far more likely to fall than those without joint problems, highlighting the critical role mobility plays in fall prevention.
13. Decreased Flexibility

With age, flexibility naturally declines, making it tougher to twist, bend, or reach out to break a fall.
Stiff muscles and tendons reduce the body’s ability to recover from a stumble.
According to Harvard Health, regular stretching routines can help maintain flexibility and, importantly, lower the risk of falls in older adults.
14. Slower Nerve Conduction
Aging causes nerve conduction to slow down, meaning signals from the feet and legs take longer to reach the brain.
This delay can blunt reflexes that are vital for maintaining balance and reacting to slips.
The National Institute on Aging explains that these slower transmissions increase the risk of falls, as the body simply can’t respond as quickly as it once did.
15. Fear of Falling

The fear of falling is a powerful psychological factor for many older adults.
This anxiety can lead to muscle tension and a reduction in day-to-day movement, ironically increasing fall risk.
Reduced activity weakens muscles and balance, fueling a vicious cycle.
As Psychology Today points out, addressing this fear is crucial for maintaining both confidence and physical stability.
16. Poor Footwear Choices

Wearing ill-fitting shoes or those with slippery soles can dramatically increase fall risk, especially for seniors with foot deformities or swelling.
Supportive, non-slip footwear is essential for safe mobility.
The American Podiatric Medical Association emphasizes that proper shoe selection is a simple yet critical step in preventing dangerous falls.
17. Environmental Hazards

Everyday surroundings can pose serious risks for older adults.
Cluttered walkways, loose rugs, poor lighting, and uneven floors all increase the likelihood of a fall—especially for those already struggling with balance.
Fortunately, simple changes like removing tripping hazards, adding grab bars, and improving lighting can make a big difference.
The CDC recommends these home modifications as effective strategies for fall prevention.
18. Cognitive Decline

Mild cognitive impairment and dementia can sharply reduce attention span and hazard awareness, making falls much more likely.
Older adults with cognitive decline often miss environmental risks or forget to use assistive devices.
The Alzheimer’s Association notes that those living with dementia are at least twice as likely to fall as seniors without cognitive issues, underscoring the importance of supportive care and supervision.
19. Alcohol and Substance Use

Alcohol and certain drugs can severely impair judgment, coordination, and reaction time, all of which are critical for fall prevention.
Older adults are more sensitive to these substances, meaning even small amounts can have a pronounced effect.
The National Institute on Aging stresses that substance use compounds existing balance issues, further elevating the risk of dangerous falls in those over 65.
20. Poor Nutrition and Dehydration

Malnutrition and dehydration are common but often overlooked in older adults.
Both can cause muscle weakness, dizziness, and confusion, all of which dramatically increase the risk of falling and sustaining injuries.
The National Council on Aging highlights that proper hydration and balanced nutrition are vital for maintaining strength, stability, and overall safety in seniors.
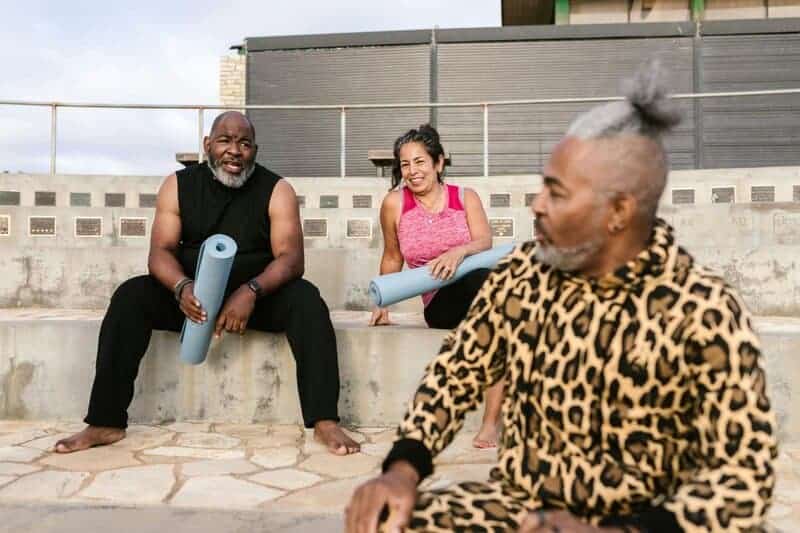
21. Reduced Physical Activity

A sedentary lifestyle often leads to deconditioning, with weakened muscles and declining balance.
This not only accelerates frailty but also increases the likelihood of falls.
Active seniors, in contrast, maintain stronger muscles and better coordination, protecting themselves from injury.
The World Health Organization stresses that regular movement is crucial for seniors, breaking the cycle of inactivity and reducing fall risk.
22. Social Isolation

Social isolation doesn’t just impact mental health—it also increases fall risk.
Those who live alone often move less, miss out on regular safety checks, and may have no one to assist them immediately if they do fall.
The National Institute on Aging notes that isolation can lead to worse outcomes and more complications after a fall.
23. Inadequate Preventive Care

Regular preventive care is crucial, yet many older adults miss out on checkups or ignore emerging health issues.
Unaddressed vision or hearing problems and skipped screenings allow hidden fall risks to go unnoticed.
The CDC stresses that early detection and intervention—through routine medical visits—are essential for reducing falls and catching problems before they turn dangerous.
24. Delayed Emergency Response

For seniors who live alone or lack access to medical alert systems, a fall can mean waiting hours before help arrives.
Longer times spent immobilized on the ground greatly increase the risk of complications like dehydration, pressure sores, or even death.
According to NIH MedlinePlus, quick emergency response is vital for improving outcomes after a fall.
25. Gender Differences in Fall Outcomes

There are notable gender differences in the consequences of falls.
Women, due to lower bone density and hormonal changes after menopause, are more likely to suffer hip fractures.
Conversely, men tend to have higher mortality rates following a serious fall.
The National Institutes of Health notes these differences stem from both physiological and hormonal factors, highlighting the need for tailored prevention strategies.
26. The Importance of Tailored Prevention

Recognizing the diverse reasons why falls become deadlier after 65 is key to effective prevention.
Personalized plans should address exercise routines for strength and balance, regular medication reviews, and home safety modifications.
A multi-disciplinary approach—involving doctors, physical therapists, and caregivers—can make all the difference.
The CDC STEADI initiative encourages comprehensive strategies tailored to each individual’s unique risks and needs.
Conclusion

The science behind why falls become deadlier after 65 is complex and deeply interconnected.
Biological, neurological, and environmental factors all contribute—but with awareness, these risks can be managed.
Proactive steps—from exercise to medication checks and home adjustments—truly matter.
Seek professional guidance for a prevention plan tailored to your needs.
Even small changes, when made early, can significantly reduce the danger of falls and help seniors maintain independence and quality of life.
Medical Disclaimer

This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment.
Always consult your healthcare provider for personalized guidance and recommendations.
Stay informed—and take proactive steps to protect your health and safety.


Vielleicht interessiert es Sie:
13 Extraordinary Giants Ready to Blow Your Mind! 🌍
10 Chonky Oddities That Will Leave You Speechless! 🤯
9 Unbelievable Absolute Units That Will Leave You Speechless! 🌟
10 Colossal Creatures That Will Leave You Speechless! 🐻
12 Shocking Absolute Units You’ll Have to See! 😲
12 Epic Absolute Units That Will Challenge Your Perceptions! 🔥
Uncover the 11 Ultimate Massive Oddities That Awe! 🌍
9 Unbelievable Oddities That Redefine ‚Massive‘! 🐉💎